Post-discharge acute care and outcomes following readmission reduction initiatives: national retrospective cohort study of Medicare beneficiaries in the United States
BMJ 2020; 368 doi: https://doi.org/10.1136/bmj.l6831 (Published 15 January 2020) Cite this as: BMJ 2020;368:l6831Linked Opinion
Evaluating the impact of incentives to reduce readmission rates in the US
- Rohan Khera
, cardiology fellow1,
- Yongfei Wang, lecturer and senior statistician2 3,
- Susannah M Bernheim, assistant clinical professor and director4 5,
- Zhenqiu Lin, senior research scientist and statistician2 3,
- Harlan M Krumholz
, professor and director2 3 6
- 1Division of Cardiology, University of Texas Southwestern Medical Center, Dallas, TX 75219, USA
- 2Section of Cardiovascular Medicine, Department of Internal Medicine, Yale School of Medicine, New Haven, CT, USA
- 3Center for Outcomes Research and Evaluation, Yale-New Haven Hospital, New Haven, CT, USA
- 4Section of General Medicine, Department of Internal Medicine, Yale School of Medicine, New Haven, CT, USA
- 5Quality Measurement Programs, Center for Outcomes Research and Evaluation, Yale-New Haven Hospital, New Haven, CT, USA
- 6Department of Health Policy and Management, Yale School of Public Health, New Haven, CT, USA
- Correspondence to: R Khera rohankhera{at}outlook.com (or @rohan_khera on Twitter)
- Accepted 14 November 2019
Abstract
Objectives To determine whether patients discharged after hospital admissions for conditions covered by national readmission programs who received care in emergency departments or observation units but were not readmitted within 30 days had an increased risk of death and to evaluate temporal trends in post-discharge acute care utilization in inpatient units, emergency departments, and observation units for these patients.
Design Retrospective cohort study.
Setting Medicare claims data for 2008-16 in the United States.
Participants Patients aged 65 or older admitted to hospital with heart failure, acute myocardial infarction, or pneumonia—conditions included in the US Hospital Readmissions Reduction Program.
Main outcome measures Post-discharge 30 day mortality according to patients’ 30 day acute care utilization; acute care utilization in inpatient and observation units and the emergency department during the 30 day and 31-90 day post-discharge period.
Results 3 772 924 hospital admissions for heart failure, 1 570 113 for acute myocardial infarction, and 3 131 162 for pneumonia occurred. The overall post-discharge 30 day mortality was 8.7% for heart failure, 7.3% for acute myocardial infarction, and 8.4% for pneumonia. Risk adjusted mortality increased annually by 0.05% (95% confidence interval 0.02% to 0.08%) for heart failure, decreased by 0.06% (−0.09% to −0.04%) for acute myocardial infarction, and did not significantly change for pneumonia. Specifically, mortality increased for patients with heart failure who did not utilize any post-discharge acute care, increasing at a rate of 0.08% (0.05% to 0.12%) per year, exceeding the overall absolute annual increase in post-discharge mortality in heart failure, without an increase in mortality in observation units or the emergency department. Concurrent with a reduction in 30 day readmission rates, stays for observation and visits to the emergency department increased across all three conditions during and beyond the 30 day post-discharge period. Overall 30 day post-acute care utilization did not change significantly.
Conclusions The only condition with increasing mortality through the study period was heart failure; the increase preceded the policy and was not present among patients who received emergency department or observation unit care without admission to hospital. During this period, the overall acute care utilization in the 30 days after discharge significantly decreased for heart failure and pneumonia, but not for acute myocardial infarction.
Introduction
The announcement and implementation of the US Hospital Readmissions Reduction Program (HRRP) were associated with a reduction in readmissions within 30 days of discharge for heart failure, acute myocardial infarction, and pneumonia,1234 as shown by a decrease in the overall national rate of readmissions. Concerns existed that pressures to reduce readmissions had led to the evolution of care patterns that may have adverse consequences through reducing access to care in appropriate settings.567 Therefore, determining whether patients who are seen in acute care settings, but not admitted to hospital, experience an increased risk of mortality is essential.
A question also arises about the association of the HRRP with the overall use of acute services in the 30 day post-discharge window. The reduction in readmissions could have occurred in the setting of changes that improved the recovery of patients and reduced the occurrence of clinical events needing acute care in the early post-discharge period. Alternatively, the decrease in readmissions might not have reduced the need for acute care but instead influenced clinicians to direct patients to the emergency department or observation units instead of pursuing hospital admission. The care of patients in the emergency department and observation units is appropriate only if they can be treated adequately in these settings without pursuing admission. An assessment of how outcomes of patients in these care settings have evolved is essential to mitigate concerns about the appropriateness of changes in patterns of acute care in the post-discharge period during the application of incentives to reduce readmission.
Accordingly, we determined whether the patients who sought acute care in the 30 days after discharge for heart failure, acute myocardial infarction, and pneumonia, the conditions the US Congress included in the HRRP,389 but were not admitted to hospital, had an increased risk of mortality. In particular, we investigated whether people who had a post-discharge emergency department visit that did not lead to a hospital admission had an increase in mortality, to determine whether the incentive programs reduced access to the hospital and caused harm. We examined the characteristics of patients, and the change over time, by their type of acute care in the 30 days after admission to hospital.
We also evaluated the temporal trends in the utilization of post-discharge acute care, including readmissions, observation stays, and emergency department visits. We determined whether declines in readmissions were associated with increases in other types of acute care. We tested whether differences existed over time in the need for acute care in the 30 days after discharge. We also evaluated the period from day 31 through day 90 to determine whether a difference existed after the evaluation period of HRRP, to see whether any change in practice was limited to the period covered by the incentives.
Methods
Data source
We used the Medicare Standard Analytic Files that included 100% of inpatient and outpatient claims for the years 2008-16. The study period spanned the announcement and subsequent implementation of the HRRP in 2010 and 2012, respectively.8 For each year, we included data for all fee-for-service Medicare beneficiaries aged 65 years and older who were admitted to hospital with a principal discharge diagnosis of heart failure, acute myocardial infarction, or pneumonia. The diagnoses were based on ICD (international classification of diseases) diagnosis codes that are included in the Centers for Medicare and Medicaid Services (CMS) measures for these conditions and are publicly available.10111213 Notably, the measure for pneumonia changed in 2014, but to ensure consistency we defined the study population for pneumonia across the study period by using the codes before the measure changed.12 Furthermore, the coding scheme changed from ICD-9 to ICD-10 in October 2015.14 Therefore, we used the CMS measure method that was rigorously tested for consistency in the patient population for each of three conditions across the transition.10
To align the study cohort with the population of patients under the purview of the HRRP, we excluded those who were discharged against medical advice, died during hospital admission, or did not have at least 30 days’ follow-up after discharge. The cohort was consistent with the specifications of the 30 day readmission metric of the CMS.911121315
Post-discharge acute care utilization and mortality
We used revenue center codes specific to claims submitted from observation stays and emergency department visits to identify these care settings. These included revenue center codes of 0762 and/or Healthcare Common Procedure Coding System code of G0378 for observation stays and revenue center codes of 0450, 0451, 0452, 0459, or 0981 for emergency department visits based on hospital outpatient claims data. These have been used in an outcome measure endorsed by the National Quality Forum and focused on post-discharge acute care.16 We used the Medicare denominator files to identify patients who died from any cause and determined the temporal relation of their date of death to the day of discharge from hospital.17 We defined 30 day post-discharge mortality as the proportion of patients discharged alive who died within 30 days of discharge.
Post-discharge care based patient groups
We examined post-discharge mortality in four mutually exclusive groups of patients defined on the basis of the clinical setting of post-discharge care accessed by patients in the post-discharge period. These included patients who were readmitted to the hospital within 30 days of discharge for any cause, were not readmitted but had an observation stay for any cause in the 30 day post-discharge period, neither were readmitted nor had an observation stay but visited the emergency department for any reason, and had no acute care in the 30 days after discharge (hospital admission, observation stay, or emergency department visit).
Risk adjusted rates of outcomes
To account for changes in characteristics of patients, we constructed logistic regression models with utilization of care and mortality endpoints across care settings as dependent variables and covariates included in the risk adjustment models in the CMS measures for each condition as independent variables (supplementary tables A-C). We calculated the calendar year and monthly risk adjusted rates of utilization and mortality as the ratio of the observed rate during the period and the expected rate in the period, multiplied by the unadjusted rate over the study period.9 To ensure consistency in covariates across ICD-9 and ICD-10 coding formats, as a part of the CMS measure design process, we mapped combinations of codes within each of the coding schemes to condition category codes for the covariates included in the model. The ICD-9 and ICD-10 codes included in the condition category codes, and data assessments showing consistency of condition category codes across the transition, are publicly available.10
Changes have been made in the number of codes on inpatient claims over time.1819 We pursued additional analyses to evaluate whether differences in covariate selection strategies substantively altered the results. We first used inpatient and outpatient claims over the preceding 12 month period to assess covariates. We found that restricting the additional inpatient covariates available from the expansion of codes to the same number available previously did not substantively alter the risk adjustment models.20 Nevertheless, to specifically determine how the strategy to identify covariates affects risk adjusted assessments in our analysis, we created a secondary cohort of hospital admissions with complete information on the order of inpatient claims (95% of the primary cohort) and used two covariate identification strategies, in which we combined outpatient claims over the preceding 12 months before the index hospital admission with either a fixed number of diagnoses from the claims across study period (nine secondary diagnosis codes, six procedure codes) or all inpatient codes (up to 25 diagnosis and procedure codes after expansion of inpatient code slots).
Statistical analysis
First, we evaluated calendar year and monthly rates of post-discharge care within the 30 day post-discharge period as readmissions, observation stays, and emergency department visits between 2008 and 2016 for each of the three HRRP conditions. Next, for each of the three HRRP conditions, we evaluated the average annual change in rates of care utilization across different care settings, based on ordinary least squares regression of rates of post-discharge care use—rates of readmissions, observation stays, emergency department visits, or care in any of three acute care settings—against calendar years. We used the non-parametric runs test to evaluate and confirm the linearity of calendar year trends, which evaluates the randomness of distribution of data points around the regression line (see supplementary methods).21 To better understand whether changes in patterns of care in a given post-acute care setting had progressed differently during the 30 days after discharge, we qualitatively evaluated care trends in these settings during post-discharge days 0-30 and 31-90 and whether an interaction existed between calendar year (2008-16) and post-discharge period (day 0-30 v 31-90) in analysis of covariance.
We then evaluated calendar year and monthly trends in post-discharge 30 day mortality across the four patient groups, based on whether patients were readmitted, had an observation stay only, had an emergency department visit only, or had no care in any of these settings. We noted that these calendar year trends were linear over the course of the study period on the basis of visual assessment and using the runs test. We also confirmed normality of residuals and homoscedasticity of data, to ensure that assumptions of linear regression models were satisfied. We used an interaction term for post-discharge care group and calendar year in an analysis of covariance model to evaluate whether calendar year trends in mortality were significantly different across the patient groups. We evaluated average annual changes in mortality rates across care settings, reported as the coefficient of change of the respective outcome in an ordinary least square regression with calendar year as a continuous independent variable. To evaluate the contribution of changes in mortality across individual care settings to the overall changes in mortality in the 30 day post-discharge period, we calculated the proportion of annual change in overall mortality rates that occurred across the three settings.
Next, to specifically investigate the possible associations with the announcement and implementation of HRRP with changing utilization across care settings, we constructed interrupted time series models assessing how the slope of the temporal trends in monthly rates of post-discharge care in the three acute care settings changed with the announcement and implementation of the HRRP. These analyses are consistent with the approach outlined in previous studies.1922
To evaluate whether systematic differences in patients’ characteristics were driving differences in outcomes, we evaluated differences in comorbidities and in-hospital events such as operative procedures and complications, as well as discharge disposition across these groups. We specifically evaluated whether comorbidities that are markers of debility, such as dementia, delirium, encephalopathy, pressure ulceration, and protein calorie malnutrition, varied across groups. The comorbidities were ascertained from all claims across inpatient and outpatient care settings in the year preceding the index hospital admission. The problems with the expansion of inpatient codes during this study period are mitigated with the use of comprehensive inpatient and outpatient codes. Finally, we assessed for markers for end of life care at discharge, including consultations for palliative care and discharge from hospital to hospice facilities.
We used SAS version 9.4 and Stata 14 for all analyses. The level of significance was set at 0.05. The study was reported in accordance with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) recommendations, and its checklist is included in the online supplement.
Patient and public involvement
No patients were involved in the development of the research question or the outcome measures, or in developing plans for the design and implementation of the study.
Results
During the study period, 3 772 924 hospital admissions for heart failure, 1 570 113 for acute myocardial infarction, and 3 131 162 for pneumonia occurred. Of these, 850 236 (22.5%) patients with heart failure, 274 142 (17.5%) with acute myocardial infarction, and 537 276 (17.2%) with pneumonia were readmitted within 30 days of discharge. The overall rates of observation stays and emergency department visits were 1.7% and 6.4% for heart failure, 2.6% and 6.8% for acute myocardial infarction, and 1.4% and 6.3% for pneumonia. Cumulatively, a third of all admissions—30.7% for heart failure, 26.9% for acute myocardial infarction, and 24.8% for pneumonia—received post-discharge care in any acute care setting.
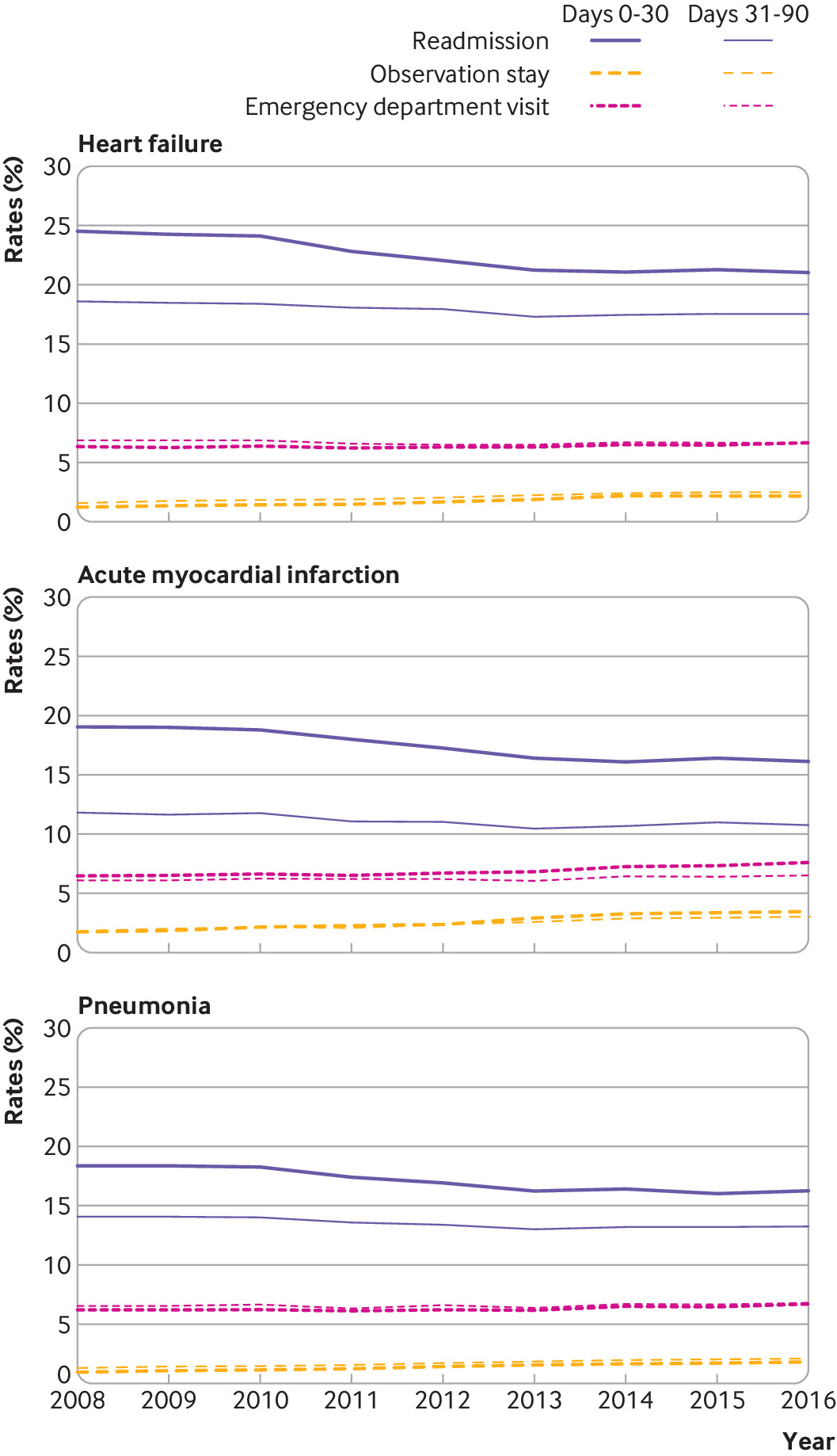
Trends in post-discharge acute care
The 30 day observed readmission rates decreased for all three conditions, from 23.5% in 2008 to 21.7% in 2016 for heart failure, from 19.0% in 2008 to 15.9% in 2016 for acute myocardial infarction, and from 17.6% in 2008 to 16.4% in 2016 for pneumonia (supplementary figure A). Risk adjusted rates followed a similar pattern, with a decrease from 24.5% to 21.0% for heart failure, 19.0% to 16.1% for acute myocardial infarction, and 18.3% to 16.2% for pneumonia (supplementary figure B). On average, risk adjusted readmission rates decreased by 0.51% (95% confidence interval −0.66% to −0.35%) per year for heart failure, 0.44% (−0.56% to −0.32%) per year for acute myocardial infarction, and 0.33% (−0.43% to −0.23%) per year for pneumonia (fig 1).
Average annual absolute percentage change in risk adjusted post-discharge care use. Coefficient for annual change derived from ordinary least squares regression. Readmissions, observation stays, and emergency department visits are mutually exclusive, presented in order of hierarchy
We observed an increase in observation stays and emergency department visits during the 30 days after discharge across the three conditions, with an average annual increase in risk adjusted rates of observation stays of 0.13% (0.11% to 0.15%) for heart failure, 0.23% (0.19% to 0.26%) for acute myocardial infarction, and 0.11% (0.10% to 0.12%) for pneumonia among patients not readmitted (P<0.001 for all). Similarly, a smaller but significant increase occurred in rates of 30 day post-discharge emergency department visits for all three conditions, with an average annual increase of 0.04% (0.01% to 0.07%) for heart failure, 0.14% (0.09% to 0.19%) for acute myocardial infarction, and 0.06% (0.02% to 0.10%) for pneumonia (P<0.001 for all) (fig 1). The combination of the increase in emergency department visits and observation stays was less than the decrease in readmissions for heart failure and pneumonia but not for acute myocardial infarction. Therefore, during this period, the overall acute care utilization in the 30 days after discharge decreased significantly for heart failure and pneumonia but not for acute myocardial infarction (fig 1).
The increase in post-discharge observation stays and emergency department visits was also apparent during days 31-90 post-discharge (fig 2). We found no significant difference between the increase in risk adjusted rates of observation stays during post-discharge days 0-30 and 31-90, across calendar years for heart failure (P=0.62) or pneumonia (P=0.50). For acute myocardial infarction, post-discharge observation stays increased in both periods, but at a higher rate during days 0-30 than days 31-90 (P for differences in slopes=0.005). Similarly, emergency department visits increased during the first 30 days post-discharge as well as in the 31-90 day period, with a larger relative increase in the early post-discharge period for heart failure and acute myocardial infarction (P for differences in slopes=0.02 for heart failure and 0.003 for acute myocardial infarction), but not for pneumonia (P=0.13).
Calendar year trends in risk adjusted post-acute care utilization during post-discharge days 0-30 and 31-90
In interrupted time series models for both unadjusted and risk adjusted assessments, monthly rates of post-discharge readmission rates decreased substantially at HRRP announcement across the three conditions (P for slope change<0.001) (fig 3; supplementary figures C-H; supplementary tables D-I) and continued to decrease at a slower rate after HRRP’s implementation. The rates of observation stays were increasing before HRRP for all conditions. They accelerated after HRRP was announced, across both unadjusted and risk adjusted assessments for heart failure. For acute myocardial infarction and pneumonia, although unadjusted observation rates did not show an inflection, conservative risk adjustment assessments suggest an increase in observation stays that was approximately a quarter of the decrease in corresponding readmission rates (P for slope change<0.05) (supplementary tables H and I). Across all three conditions, we observed no inflection in rates of emergency department visits after HRRP announcement, but a significant increase occurred after HRRP implementation that was approximately a quarter of the decrease in readmissions during this period (P for slope change<0.05).
Changes in monthly rates of risk adjusted post-acute care utilization after announcement and implementation of Hospital Readmissions Reduction Program (HRRP). Dots represent monthly risk adjusted rates of post-acute care use in individual settings; lines represent slope of change in rates during each period relative to HRRP. Interrupted time series models evaluated for changes in slopes at announcement and implementation of HRRP, demarcated by vertical lines
Mortality across post-discharge care groups
The overall post-discharge 30 day mortality was 8.7% for heart failure, 7.3% for acute myocardial infarction, and 8.4% for pneumonia. Post-discharge 30 day mortality was higher in patients with readmissions (13.2% for heart failure, 12.7% for acute myocardial infarction, and 15.3% for pneumonia) than in those with observation stays (4.5% for heart failure, 2.7% for acute myocardial infarction, and 4.6% for pneumonia), emergency department visits (9.7% for heart failure, 8.8% for acute myocardial infarction, and 7.8% for pneumonia), or no post-discharge acute care (7.2% for heart failure, 6.0% for acute myocardial infarction, and 6.9% for pneumonia).
Cumulatively, a third of post-discharge deaths occurred in people who were readmitted within the 30 day period (supplementary figure I). Among those not readmitted, most deaths within the 30 day post-discharge period occurred in people who had neither observation stays nor emergency department visits, which represented more than 60% of the overall post-discharge 30 day mortality across the conditions. Patients who were not readmitted but who received care in observation units or the emergency department represented less than 10% of all deaths in the post-discharge period (supplementary figure I).
Over the study period, risk adjusted post-discharge mortality increased from 8.4% to 8.8% for heart failure and decreased from 7.5% to 7.0% for acute myocardial infarction and from 8.3% to 8.1% pneumonia (fig 4; unadjusted rates in supplementary figure J). The increase in post-discharge mortality for heart failure began before the announcement of the HRRP. The average risk adjusted post-discharge 30 day mortality increased by 0.05% (0.02% to 0.08%) per year for heart failure and decreased by 0.06% (−0.09% to −0.04%) per year for acute myocardial infarction during 2008-16 (fig 5; unadjusted rates in supplementary figure K). Of the overall increase in mortality in patients with heart failure, increase in mortality was concentrated among people who were neither readmitted nor received care in an observation unit or an emergency department (fig 5). The rate of increase in mortality in this group without any acute care in inpatient units, observation wards, or the emergency department was 0.08% (0.05% to 0.12%) per year, rates of increase that exceeded the overall increase in post-discharge mortality in heart failure. In contrast, decrease in post-discharge mortality in patients with acute myocardial infarction was concentrated among those who were readmitted. For pneumonia, the overall mortality rates did not change over the study period. Therefore, increases in post-discharge mortality were limited to patients with heart failure who did not receive post-discharge acute care in of the three settings.
Risk adjusted rates of death in the 30 day post-discharge period by post-discharge care use, 2008-16. Points represent proportion of patients discharged alive who died in 30 day post-discharge period, based on post-discharge acute care utilization
Average annual absolute percentage change in risk adjusted 30 day post-discharge mortality by post-discharge care use. Coefficient for annual change derived from ordinary least squares regression. Readmissions, observation stays, and emergency department visits are mutually exclusive, presented in order of hierarchy
We observed no effects of the announcement or implementation or HRRP on temporal trends in mortality among patients who received post-discharge acute care in observation units or the emergency department. Specifically, in interrupted time series models that evaluated for the effects of mortality, across all three conditions and for unadjusted as well as risk adjusted assessments, no HRRP associated inflections in mortality occurred in these settings at either the announcement of the HRRP or its implementation (fig 6; supplementary figures L-Q; supplementary tables J-O). This suggests that the HRRP was not associated with an increase in mortality risk among patients receiving care in observation units or the emergency department in the post-discharge period.
Changes in slopes of monthly rates of risk adjusted post-discharge mortality across groups of post-discharge acute care utilization after announcement and implementation of Hospital Readmissions Reduction Program (HRRP). Dots represent monthly risk adjusted rates of post-acute care use in individual settings; lines represent slope of change during each period relative to HRRP. Interrupted time series models evaluated for changes in slopes at announcement and implementation of HRRP, demarcated by vertical lines
Characteristics of patients by post-discharge care setting and outcomes
We observed differences in markers of frailty and advanced healthcare needs between groups depending on whether they survived to post-discharge day 30 or died after seeking post-discharge care in various settings (table 1, table 2, table 3; supplementary tables P-R). Across all conditions, patients who died had a higher prevalence of markers of debility including dementia, functional disability, delirium, chronic skin ulceration, and protein calorie malnutrition. Among deceased patients, the prevalence rates of these conditions were substantially higher in those who died without having used any post-discharge acute care (table 1, table 2, table 3). Those who died also had a higher rate of markers of advanced disease such as cardiorespiratory failure, metastatic cancer, and acute leukemia; however, these markers did not differ between groups based on their post-discharge care use. Furthermore, the group of patients without post-discharge acute care use had much higher rates of palliative care consultations and discharge to hospice facilities. In the group of patients who died without using post-discharge acute care, 19.4% with heart failure, 21.0% with acute myocardial infarction, and 17.0% with pneumonia had a palliative care consultation before discharge. Notably, whereas 3.6% of patients with heart failure, 3.2% of patients with acute myocardial infarction, and 3.1% of patients with pneumonia were discharged to a hospice following the index hospital admission, among patients who died without using post-discharge acute care, 45.3% with heart failure, 49.1% with acute myocardial infarction, and 42.0% with pneumonia had been discharged to a hospice after the index hospital admission.
Characteristics of patients with heart failure according to survival and post-discharge acute care use. Unless stated otherwise, numbers represent proportion of patients discharged alive with heart failure
Characteristics of patients with acute myocardial infarction according to survival and post-discharge acute care use. Unless stated otherwise, numbers represent proportion of patients discharged alive with heart failure
Characteristics of patients with pneumonia according to survival and post-discharge acute care use. Unless stated otherwise, numbers represent proportion of patients discharged alive with heart failure
We also saw disease specific temporal trends in discharges to hospice facilities. Across all patients, 3.6% with heart failure, 3.2% with acute myocardial infarction, and 3.2% with pneumonia were discharged to a hospice, with an increase in these discharges in heart failure and pneumonia but not in acute myocardial infarction (fig 7).
Trends in discharge to hospice. Discharge to hospice by calendar years across patient groups based on their post-discharge care utilization
Discussion
Between 2008 and 2016, although the national readmission rate decreased significantly across all three conditions included in the HRRP (heart failure, acute myocardial infarction, and pneumonia), the use of emergency departments and observation units significantly increased. The decline in readmission rate was greater than the rise in the use of other acute care settings. Therefore, overall post-discharge acute care—representing the aggregate of readmissions, observation stays, and emergency department visits—decreased for patients with heart failure and pneumonia but not for patients with acute myocardial infarction. Patients receiving post-discharge care in the emergency department and observation units who were not readmitted had lower mortality than did those who were readmitted. Most deaths in the 30 days after discharge occurred in patients who did not seek any post-discharge acute care, with less than 10% occurring in those with post-discharge care in observation units and emergency departments. During this period, which ran from before the HRRP through the its announcement and implementation, only patients with heart failure had a significant increase in post-discharge mortality, which began before the announcement of HRRP. The increase, however, was almost exclusively observed among patients without post-discharge acute care and was not a result of deaths among those with emergency department visits or observation stays who were not admitted. Nearly half of all patients who died without any post-discharge acute care had been discharged to a hospice from the index hospital admission.
Trends in post-discharge observation stays and emergency department visits
Observation stays and emergency department visits have increasingly been used in the post-discharge period.1 We found that the rise in the care in these settings attenuated some of the reductions in readmissions during 2008-16, expanding on a similar observational analysis using Medicare data from 2012 to 2015.23 Collectively, the patterns suggest a transition in how patients receive post-discharge acute care. The MedPAC, a non-partisan organization that does analyses for the US Congress, evaluated the HRRP and similarly found reductions in readmissions with increases in emergency department and observation visits.24 Notably, we found an increase in these care settings that was not restricted to the 30 day reporting period and occurred at a similar rate during days 31-90 post-discharge. The MedPAC also found that observation stays and emergency department visits occurred among patients with conditions that were not targeted in the HRRP.24 Therefore, we cannot be sure whether the changing patterns of post-discharge acute care was part of a strategy to reduce readmissions or whether they were related to other concurrent policy changes such as the wider implementation of criteria for inpatient hospital admissions that discouraged inclusion of short hospital stays.32526 Nevertheless, the overall rise in alternative post-discharge acute care in the 30 day period requires an assessment of whether patients’ experience improved with this transition and whether avenues exist for further improvement of post-discharge care and recovery.
Outcomes in observation stays and emergency department visits
We found that patients who received care solely in observation units and emergency departments had lower rates of mortality than those who were admitted to hospital, indicating that these settings were likely utilized for patients at lower risk. Thus, the result does not support the concern that patients at high risk are denied access to the higher level services they need.56 The changes in mortality—especially for patients with heart failure, who have experienced rising post-discharge mortality—largely occurred among people who had had no post-discharge acute care utilization.
What remains unclear is whether these changes in post-discharge mortality, which were exclusively observed for patients with heart failure, represent a failure of appreciation that these patients needed acute care or a group with expected deaths in the setting of comfort centered, end of life care. We noted that this group of patients had high rates of palliative care utilization and discharge to hospice facilities. However, these observations do not completely explain the elevated mortality risk in patients who did not utilize post-discharge acute care. Moreover, although suggested in a previous study,5 patients with pneumonia have not had a consistent rise in post-discharge mortality in our more contemporary assessment.
Comparison with literature and implications for health policy
The study strongly suggests that the HRRP did not lead to harm through inappropriate triage of patients at high risk to observation units and the emergency department, and therefore provides evidence against calls to curtail the program owing to this theoretical concern.6 The concern was mainly raised by one study that ascribed a rising mortality in the period spanning the announcement and implementation of HRRP to the effects of the program, also reporting that this increase was restricted to patients who were not readmitted.5 This study, like others,9272829 found that post-discharge mortality in these conditions was increasing nearly three years before the announcement of HRRP but ascribed an excess increase to HRRP after modeling HRRP’s effects as changes across four 30 month periods discounting within period trends.5 It also used inpatient data to define case mix and used a consistent number of codes after the expansion of coding slots on inpatient claims. The conclusions of the study contrasted with those of another that also found an increase in mortality from heart failure and pneumonia during 2006-14 but did not find inflections in the slopes of monthly rates of mortality in interrupted time series models, while specifically accounting for within period trends.9 Moreover, it used inpatient, outpatient, and physician claims for risk adjustment, and used all claims data for identification of covariates after code slots expanded, without any analytic differences emerging owing to covariate selection strategies. Interestingly, a recent study by the authors whose initial study suggested a rise in mortality for heart failure and pneumonia in Medicare following implementation of HRRP found no changes in mortality for these conditions after modeling them as monthly changes during 2012-15,23 despite including the same study population and the same data. The study also did not report mortality rates in observation units and emergency departments, despite a focus on the care in these settings.23
Other studies using national Medicare data have focused on temporal trends in subgroups of hospitals and patients and are, therefore, not directly comparable to the above studies focusing on overall trends.3031 Finally, an analysis using 100 000 hospital admissions among Medicare beneficiaries in a quality improvement registry drawn from 500 US hospitals, which captured an inconceivably low two admissions for heart failure on average per hospital per month, did not replicate the secular trends in heart failure readmissions or mortality nationally.2232 It thus cannot form the basis of generalizable conclusions about the effects of the program.32 The reassuring findings from our study complement hospital level assessments, which have found that reductions in readmissions are on average associated with reductions in mortality.33 No evidence has been found to support the hypothesis of gaming of quality measures by delaying or deferring readmissions, as no discontinuities in readmission or mortality are seen around day 30.34
Our study also explores other potential concurrent changes in patient care, such as end of life care, that may be reflected in post-discharge outcomes. However, whether markers of debility or end of life care need to be considered in measures cannot be directly inferred. Rates of these illnesses among patients who are readmitted are low, and, because they are potentially related to the quality of in-hospital care processes, excluding them in the assessment of readmission measures may not be appropriate. Finally, the current mortality measures were designed with considerations for such care needs before the index hospital admission, and patients receiving hospice care were excluded from the measure population.3536 These measures focus on post-admission 30 day mortality, which captures the entirety of the care experience of patients during the hospital admission and in the post-discharge period. Hospitals, therefore, focus on this composite of mortality. The current discussion about HRRP has exclusively focused on post-discharge mortality, despite a notable concurrent trend for reduction in in-hospital deaths, which have reduced at a rate comparable to the rise in post-discharge deaths. An independent assessment by MedPAC also found that risk adjusted cumulative in-hospital and post-discharge 30 day mortality have slightly decreased over the period spanning the introduction of the HRRP.337
Limitations of study
Our study has some limitations. We were unable to identify patterns of acute care during the index hospital admission that would be associated with a higher rate of post-discharge acute care in observation units and emergency departments and whether these visits represented avenues for planned post-discharge follow-up care. Moreover, the proportion of these care encounters that were preventable remains poorly understood. Next, our assessment of discharge destination is exploratory and does not track the patient’s location in the post-discharge period. Finally, we were unable to elucidate the cause of death among patients who did not seek post-acute care but died after a hospital admission owing to our use of deidentified data. However, this is unlikely to represent refusal of care, as there are specific laws against refusal of care to acutely ill patients requesting emergency care. Moreover, current quality measures do not disincentivize care in the emergency department or observation units, and no incentives exist for hospitals to refuse acute or emergent care. Also, our study focuses on all US hospitals and not merely the hospital with the index admission, and the other hospitals do not have a reason to refuse needed care. An investigation into these deaths remains important.
Conclusion
Among patients admitted to hospital with conditions targeted in the HRRP, a recent decrease in readmissions is balanced by an increase in observation stays and emergency department visits in the 30 days after discharge, such that the overall post-discharge acute care utilization has remained unchanged. However, we found no evidence for harm related to increasing care in alternative acute care settings, and patients who received care in observation units or emergency departments and were not readmitted had low rates of post-discharge 30 day mortality and were not affected by the announcement or the implementation of the HRRP.
What is already known on this topic
With incentives to reduce readmission rates in the US, patients who need hospital admission after a recent discharge may be denied access, which would increase their risk of mortality
Among Medicare beneficiaries admitted for heart failure, mortality in the 30 day post-discharge period has been increasing over the past several years
Observation units and emergency departments have increasingly been used as avenues for patient care in the US
Data on utilization of these services soon after discharge for conditions targeted in the Hospital Readmissions Reduction Program (HRRP), and patients’ outcomes, are needed to evaluate the effects of the program
What this study adds
Among conditions targeted in the HRRP, patients with heart failure, but not those with acute myocardial infarction or pneumonia, experienced an increase in post-discharge 30 day mortality
This increase preceded the announcement of the program and was concentrated among patients who sought no post-discharge acute care, nearly half of whom had been discharged to a hospice
Despite increasing utilization of observation units and emergency departments in the post-discharge period, care in these settings was not associated with increased mortality risk
Footnotes
Contributors: All authors were responsible for the study concept and design. RK, YW, and HMK were responsible for the acquisition and analysis of data. All authors contributed to the interpretation of the data. RK drafted the manuscript. All authors critically revised the manuscript for important intellectual content and approved the final version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. The study was conceived and conducted by the authors, and the Centers for Medicare and Medicaid Services played no role in its design and conduct; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. RK and HMK are the guarantors.
Funding: RK is supported by the National Center for Advancing Translational Sciences (UL1TR001105) of the National Institutes of Health. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: support from the National Center for Advancing Translational Sciences (UL1TR001105) of the National Institutes of Health for the submitted work; HMK is a recipient of a research grant, through Yale, from Medtronic and Johnson and Johnson (Janssen) to develop methods of clinical trial data sharing; HMK was a recipient of a research grant, through Yale, from Medtronic and the Food and Drug Administration to develop methods for post-market surveillance of medical devices; HMK was a recipient of a research agreement, through Yale, from the Shenzhen Center for Health Information for work to advance intelligent disease prevention and health promotion, and collaborates with the National Center for Cardiovascular Diseases in Beijing; HMK received payment from the Arnold and Porter Law Firm for work related to the Sanofi clopidogrel litigation and from the Ben C Martin Law Firm for work related to the Cook IVC filter litigation; HMK chairs a cardiac scientific advisory board for UnitedHealth and is a participant/participant representative of the IBM Watson Health Life Sciences Board; HMK is a member of the Advisory Board for Element Science, the Physician Advisory Board for Aetna, and the Advisory Board for Facebook; HMK is the founder of Hugo, a personal health information platform. HMK, SMB, ZL, YW work under contract with the Centers for Medicare and Medicaid Services to develop and maintain performance measures that are publicly reported; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The study was reviewed by the Yale University Institutional Review Board and deemed exempt from informed consent owing to the use of deidentified data.
Data sharing: The data are proprietary to the Centers for Medicare and Medicaid Services and can be obtained from them directly. The statistical code is available from the corresponding author.
The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: The data are de-identified and, therefore, cannot be shared with the study participants directly. The authors will enlist patient and public participation in the dissemination of the results of the study.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.